My Bra Died- But, I Survived Respiratory Distress and Sepsis
The day my bra died: I had plans to enjoy watching my grand daughter’s skating lesson I had no idea my life would turn on a dime that Saturday. Respiratory distress can happen to any one, particularly the very young; those with chronic lung conditions and those over age 65. Today I was the one who had an life threatening event.
I felt awful when I woke up at 2 AM that day. But, I still was still trying to putter around. This blog shares some personal details about why ER staff had to cut off my clothes on a recent Saturday. I encourage you my readers to think about what IF you were in a similar medical crisis. What would you do?

I got citicaly ill so quickly. The ER staff had to cut my clothes off. This is waht was left of my best bra, new sweater jacket and tank top. But I survived acute respiratory distress with hypoxia.
I could not put my finger on it.I was thinking I had a repeat sinus infection. My face was cherry red. I had been complaining of aspiration all too often.
Since I don’t drive I called Dispatch, a local Mobile Urgent Care Provider in Colorado Springs. There were to arrive at my door around 12:30.
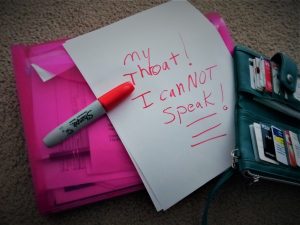
I was in acute repiratory distress. I could not utter a sound. I could not speak- sign of repiratory distress a 911 emergency.
Speechless
I had prepared to pay my co-pay, show my insurance card, my medication list. my doctors’ names and my CODE STATUS as DNR etc to the PA and Paramedic that were coming from Dispatch Mobile Urgent Care. I had written down my symptoms, which were not significant at all at the time.
I went to the bathroom before they arrived. Leaving the bathroom I heard them knock on the door. I tired to say, “Come in,” as I approached the door but no sound came out of mouth.
I was speechless.
As the two men walked into my home, I held my hands to my throat. ( Universal sign that a person can not breathe.)
I grabbed a pen and paper to write messages to the urgent care providers. I was not choking, but my air way had closed up: a life threatending event.( My images above are after-the fact.)
The universal sign for choking is hands clutched to the throat. If the person doesn’t give the signal, look for these indications:
- Inability to talk
- Difficulty breathing or noisy breathing
- Squeaky sounds when trying to breathe
- Cough, which may either be weak or forceful
- Skin, lips and nails turning blue or dusky
- Skin that is flushed, then turns pale or bluish in color
- Loss of consciousness
Please read the full article from Mayo Clinic. Knowing what to do quickly may save a life. This article is anecdotal: not meant to be medical advice.
My throat had been spasming and losing my voice with increased frequency over that few weeks. I had been receiving medical care and under going tests…lots of tests… to determinine why I was loosing function on my right side. I knew all of this was related to what ever was going on with me. I was worried and wanted to prevent aspiration pneumonia after inhaling liquids and food particals so often. ( Up coming post will share about my respiratory appointments at National Jewish Hospital in Denver.)
Aspiration pneumonia
Aspiration pneumonia occurs when you inhale food, drink, vomit or saliva into your lungs. Aspiration is more likely if something disturbs your normal gag reflex, such as a brain injury or swallowing problem, or excessive use of alcohol or drugs.
Complications
- Bacteria in the bloodstream (bacteremia). Bacteria that enter the bloodstream from your lungs can spread the infection to other organs, potentially causing organ failure.
- Difficulty breathing. If pneumonia is severe have chronic lung diseases… you may have trouble breathing in enough oxygen…. hospitalized and use a breathing machine (ventilator) while your lung heals…
I am talking abut serious stuff here...Please read the entire article from Mayo Clinic to be better informed more of the potential compliction of aspiration pneumonia. https://www.mayoclinic.org/diseases-conditions/pneumonia/symptoms-causes/syc-20354204
At this point when basic urgent medical care was at my door, my air way had shut off. I was suddenly in acute distress. I happened so fast.
- The two trained medical professionals knew by looking at me that I was in trouble.
- While one took my vital signs the other one called 911 for emergency transport.
I was extremely week, but I wanted to gather my stuff…I’m no pansey! I have alwasy been the rescuer rather than the victim.
Within minutes my apartment was filled with people wearing big fire men coats and others wearing uniforms. ( I thought, I have dirty idsshes in the sink.) They got me on a gurney then took me thorugh the patio door to the parking lot where a fire truck and ambulance were waiting. I heard my neighbors wishing me well.
In inside the ambulance, some one told me, “Malika open your eyes. come on…open your eyes.” I could understand the urgency in the voice.
I struggled to open an eye. ” Open your eyes…we may have to *tube her.” ( I was thinking that I wanted to tell them they my right eye lid muscles do not work. I have blephrospasms. Sometimes my eye lids clamped closed. Taht I why I am getting very specailize neuorlogical care.)
I felt some one pick up my left hand. I briefly open an eye that signal my rescuers I was still with them…sort of…
When I had my eye opened I sawa my left hand that they were starting on IV in was really, really , really BLUE. I wanted to point out that fact to the paramedics. I wanted say, ” My hand is blue.” But, I still could not speak.
Besides they had a O2 cannula in my nose then at some point a Bi-pap over my nose and mouth that forced air into me.
I only live 2 miles from the closest hospital. Normally it is a 10 to 15 minute taxi ride. I had no o of the trip other than the commands ” Malika! Open, your eyes for me…open your eyes.” I did not want to open my eyes, but some one inisitantly shaking my shoulder.
I remember the rush of cold air as gurny left the ambulance with me strapped to it.
Then voices again were telling me, MALIKA! Open your eyes…Get ready to tube her.” I knew what that meant. They were about to intubate me. I was so weak I did not care if they put an artificial airway or not. I opened my eyes to see at least a dozen people in a room waiting for me.
* Tracheal intubation, usually simply referred to as intubation, is the placement of a flexible plastic tube into the trachea (windpipe) to maintain an open airway or to serve as a conduit through which to administer certain drugs. It is frequently performed in critically injured, ill, or anesthetized patients to facilitate ventilation of the lungs, including mechanical ventilation, and to prevent the possibility of asphyxiation or airway obstruction. https://en.wikipedia.org/wiki/Tracheal_intubation

Recovery with CPAP and O2 post acute respiratory distress reenctly. My hair is n’t combed and I did not care. See post on my experince with severe respiratory infection and ER care
Life Saving Pioritities
“MALIKA, we are going to cut off you clothes to get an XRAY and get some IV lines and medication in you..”
I thought, “CRAP! That is my new sweater jacket. OMG! I am wearing my best bra..NO-O-O-O-O-O-O!” But I could not speak. I had no strength to resist the medically necessary action. AS an old RN, I knew they did what they had to do, but still…I just bought that nice sweater.
I had so many people working on me. I heard some one tell me they were doing an ABG (arterial blood gas). Some one else said, “I’m starting another line in your right hand.” ( Intravenous neede inserted into the vein to infuse fluids.)
I heard some one say, ” Her WBC is 27. lactate is 4.” I knew they were talking about my White Blood Cell Count YIKES! I had an infection! I knew what Lactate was in the ER, but still my brain thought of “lactating mothers”…I had worked in OB for years, but the terms meanings are not the same.
Sepsis is a life-threatening condition that arises when the body’s response to infection causes injury to its own tissues and organs.[8] Common signs and symptoms include fever, increased heart rate, increased breathing rate, and confusion …..https://en.wikipedia.org/wiki/Sepsis
Power and Control
The ER staff was in charge.
I could hear what was going on in the ambulance and the ER. I could not respond except to work hard to open a eye now and then. I appreciated everyone talking to me and telling me what they were doing.
I could NOTHING to help myself, yet, the staff who so professionally spoke to me telling me what they were doing made me feel safe and secure with some remaining elements of me still have some kind of power and control over my own life at a point when I desperately needed help.

IV pump machnes with tubes adn bags of lfuid hanging may look scary. But, gratefully people today can get fluid support and medically necessary medications very quckily via IV into a vein.
Thank You!
I want to say Thank you to the Colorado Springs Dispatch Mobile Urgent Care crew, AMR paramedics, and the Memorial Hospital Central ER staff who worked like a wheel oiled machine to save my life April 7, 2018.
I survived acute respiratory distsress and whopping infection; sepsis, because of the quick action of local Colorado Springs medical professionals.
Note: my disabled son wears a “I’ve fallen and can’t get up button for himself. Unfortunatley, that emergency call system is extremely unsatfisfactory in responce time. 5 to 10 minutes to answer if at all. If the urgent care team had not been in our home when my airway closed up the resoonce time would have been too late.
This blog post is plently long and I sitll want to typo a big thank you to Memorial Hospital Med Surg staff in Colorado Springs for their wonderful inpatitent care while I was hospitalized. ( Special thank you to Mary. You know who you are.)
That experience will be in a post following. I want to address a few more medical issues for my readers to begin thinking about for themselves.
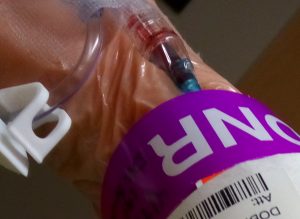
Do you have your advanced medical directives in writing? My wish is for no extra ordinary heroic measures to keep me alive. My CODE status is DNR Do Not Resusuitate. See blog post for my why.
My Advance Medical Directives: DNR
No matter your age or medical history everyone needs to have an Advance Medical Directive in place. If you do not yet, my readers, please start talking about and writing out your emergency wishes for medical care TODAY!
I have papers plasterd on my refrigerator about medications; my Advanced Directives; my doctors; my allergies and my individual medical conditions that will affect my care in the owrst case scenario..
IF and when a para medic or fire department answers a call they will look at the refigertor door to see if ther are any notes about medical directions. Dear readers, if you don’t already have important medical information on your refrigerator door for every member of your family, please do so before you go to bed tonight. That handy information may save a life.
What’s this about DNR?
Decades ago my sisters and I had soem serious discussions after our mother suffered her first strokes. Medical staff asked our father what he and mother would want to do if her heart stopped. Our parents really had never talked about. Our dad, quite frankly was totally clueless to anything medical. In fact few healthy people ever think about what IF an accident happens?
Intubating me while still alive with a heart beat would have been fine. But if my heart stopped, I do not want any heroic efforts beyond a little effort to make me come back to life then keep me in a state of ‘not really living’. I have chosen DNR to take the burden off of any staff and my family frm having to make a tough call and always wonder, ” Did I make enough effort? Did I make the right choice to stop CPR?”
My wish is to do what you can can…then let me go in peace. I can not make that decsison for you, dear readers. I want you to please think about the unthinkable. Have a plan of action so you don’t put any more stress on your family by having prepared no last wishes.
I know I was near death on April 7th. I was in no pain. NO white light. No guardina angel calling me home. I did hear the voices of people helping me and that gave me peaceful confidence when I could not care for myself…the white lights were medcially necesasry in the ER… they followed protocol to support my breathing properly. If my heart had stopped my DNR records on my medical chart ; my wallet and posted on my frig relieved rescuers of responcibility to do extra ordinary measures to keep my body alive, except fo organ transplant or for research donation.
I am still recovering from a nasty upper respiratory infection, but I really wanted to get my thoughts typo’ed asap.That is enough to think about for today.
Views: 707
