This Week is National Poison Prevention Week (March 20-24, 2023)
Today, March 20, 2023, marks the first day of This National Poison Prevention Week (March 20-24, 2023). I encourage everyone to take this moment to set aside at least 5 minutes every day to take a close look at the potential for poisoning in your home. In families with small children, the amount of dedicated time needed will obviously take longer to peruse your home.
In this post, No Non-cents Nanna shares the Press Release from the CPSC, The U. S. Consumer Product Safety Commission. I’ll share some safety tips: how and where to get help if someone is suspected of swallowing poison; common poisonous materials that children accidentally put in their mouths including ,medications, lithium batteries and seasonings in your kitchen cupboard.
You’ll be surprised, I guarantee. For those who want to hold out to the end of this post/ video, I some a BONUS for you.
Get the gears in your head turning as we examine Child-Safety and Poisoning more closely. We’ve got some critical thinking to do…
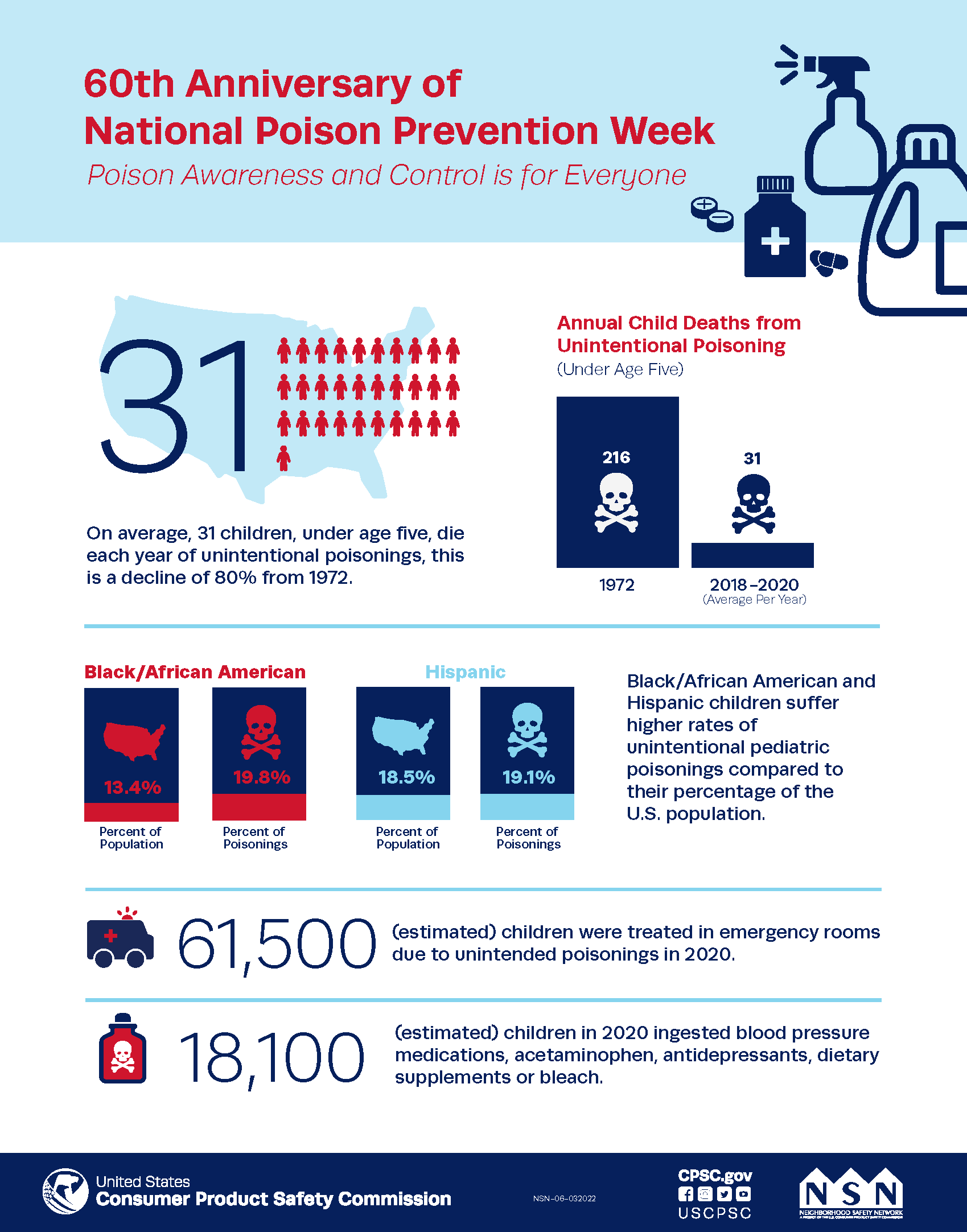
It was not until 1972 that the U. S. governmental agency began to require “child-proof” packaging. According to the CPSC, Child poisoning deaths have fallen by 73 percent since 1972 due to tough federal laws including the Poison Prevention Packaging Act (PPPA) of 1970 and the Child Nicotine Poisoning Prevention Act of 2015, and the cooperation of the poison prevention community.
On a personal Note:
That’s a picture of me when I was three. All sweet and innocent with the curiosity of a cat, poking my nose into anything and everything.
I remember vividly using the bathtub side to help me climb up into the bathroom sink for an orange-flavored snack from the medicine cabinet.- a big bottle of baby aspirin. I was generous to share a few with my older sister after I had eaten most of the bottle by myself.
My sister, age five, thought I wasn’t being fair with her, so she tattled on me for eating all of the orange stuff That tattle tell is the only reason my mother found out what I had done – this time. I remember old Doc Mccreedy shoving a tube down my throat – I fought it. I fought hard. I bit the tube. He gave up.
My mom was mad – really mad – so she called her father – my “daddy” was away with the National Guard. My grandfather rode the bus to come to watch me for a time while my mom worked. Oh and was Grandpa mad – he was not angry with me, only being 3. He was angry at my mother for leaving me alone in an upstairs apartment.
Back in the 1950s baby medicine came in big bottles – in quantities larger than should be used before expiring – with screw-on lids that even a 3-year-old could open all by themselves.
I still remember my immature confusion. I was hungry. I thought my mommy would be proud of me for not bothering her when I was hungry. It took me a few more years to figure out all of that.
My point is that children do not think as adults do. Grownups cannot assume that children know what is safe and what is not safe. Until a child is more mature, it is up to parents, or other childcare providers to protect the innocent as they explore their surroundings and test their boundaries. It is natural for children to explore by putting things into their mouths. (Consider developmental stages.)
According to National Electronic Injury System are the most common unintentional poisoning items.
- Blood Pressure Medication.
- Acetaminophen
- Bleach
- Ibuprofen
- Anti-depressants
- ADHD medication
- Laundry Packets
- Dietary Supplements
- Diphenhydramine
- Unknown
Source: National Electronic Injury System June 2020
SAFETY TIPS:
Remember: “An ounce of prevention is worth a pound of cure.”
Remember and recheck that you have stored potentially poisonous material locked away and or up high away from small children.
The Hazard Analysis staff searched NEISS databases for all incidents with poisoning diagnoses (code 68)
or chemical burn diagnosis (code 49) involving children under the age of 5.
They found that not all poisonings were from carelessly leaving pill bottles within the child’s reach but were from “allergic” or “adverse” reactions or “fumes” that we hope does not happen or from caregiver error in the amount given “or an unforeseen incidental exposure from a situation beyond the victim’s control.
In other words, the tot did not choose to ingest in the process of exploring. The 3rd situation, incidental exposure makes me angry.
1. Adverse Reactions: This includes undesirable effects that occur with the proper use of a
substance (e.g., drowsiness after administration of an antihistamine).Allergic, hypersensitivity,or idiosyncratic reactions to recommended doses of vaccines, antibiotics, or other medications
are also included in this category.2. Therapeutic Errors: Unintentional mistakes made during a prescribed or recommended
course of treatment, such as:(1) a caregiver administering the wrong substance or an overdose
(e.g., two tablespoons instead of two teaspoons) to the patient;(2) a pharmacist mislabeling the dosage instructions on a prescription;
(3) a caregiver giving medication to the wrong child.
3. Incidental Exposures:
This category refers to exposures resulting from a situation beyond
the control of the victim.Examples include exposures to:
(1) chlorine fumes from a pool;
(2) gas fumes while in a dwelling or an automobile; (3) gasoline while it is being pumped into an automobile; or
(4) illicit drugs (e.g., cocaine, methamphetamine, marijuana) while the caregiver
is using or producing them.
Release Date: March 20, 2023 | Release Number: 23-162
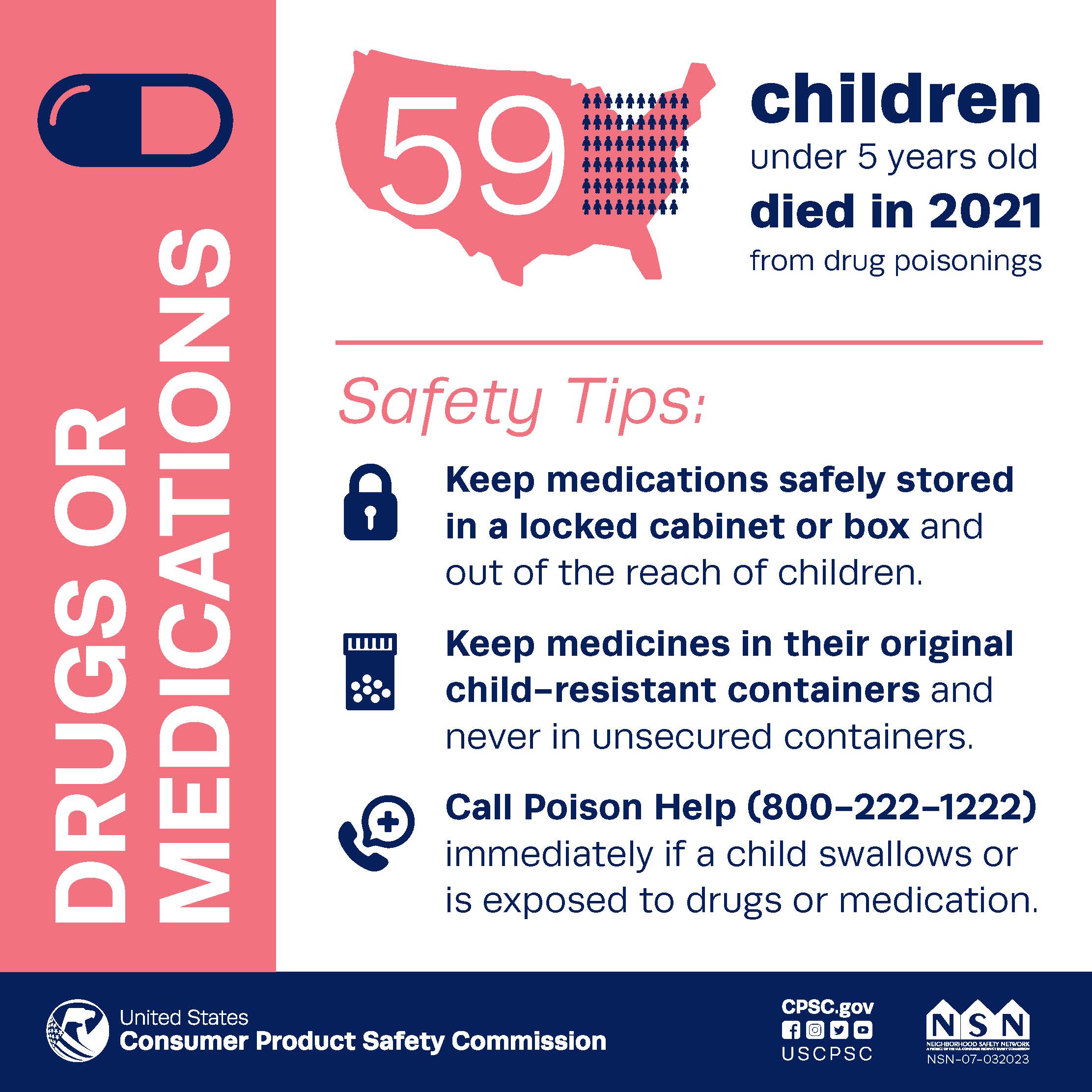
CPSC Report Finds 37 Percent Spike in Child Poisoning Deaths in 2021
WASHINGTON, D.C. – Unintentional pediatric poisoning deaths spiked 37 percent in 2021, with 59 children under five years old losing their lives after gaining access to prescribed or illicit drugs. The U.S. Consumer Product Safety Commission (CPSC) encourages consumers to safeguard their families, especially those more vulnerable, from poisonings by taking control of potentially harmful household products, medications and drugs. This National Poison Prevention Week (March 20-24, 2023) marks 61 years since the first national observation. Child poisoning deaths have fallen by 73 percent since 1972 due to tough federal laws including the Poison Prevention Packaging Act (PPPA) of 1970 and the Child Nicotine Poisoning Prevention Act of 2015 and the cooperation of the poison prevention community. This community includes the American Association of Poison Control Centers, standard development organizations, consumer advocates, medical professionals, industry and government.
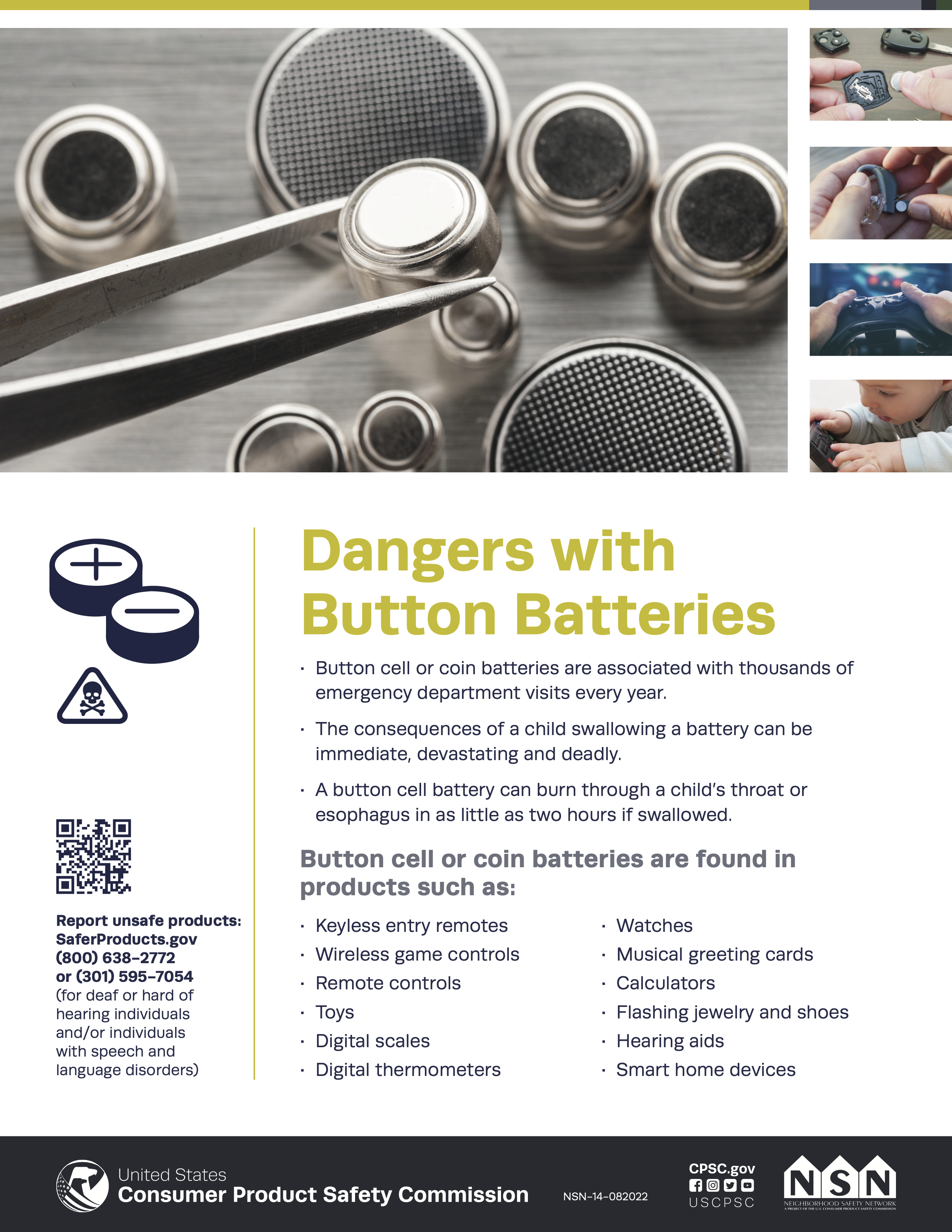
“Sadly, this report shows the work that still needs to be done to protect children,” said Alexander Hoehn-Saric, Chair of the U.S. Consumer Product Safety Commission. “Nearly eight out of 10 poisonings occurred in the home. Please take the time to store cleaning supplies, laundry packets, button batteries, and drugs out of children’s reach or in locked cabinets. If you see it lying around, a child can grab and swallow it.”
CPSC’s latest report notes that African American children suffer a higher rate of unintentional pediatric poisoning injuries, 21.4 percent, compared to being 15.8 percent of the U.S. population. The report also found that blood pressure medications, acetaminophen, antidepressants, laundry packets and bleach are the five products most involved in unintentional pediatric poisonings. CPSC encourages family members and caregivers to identify hazards in the home that could be a poisoning danger and keep them out of a child’s sight and reach.
Safety tips for parents and caregivers:
Drugs or Medications
- Keep medications safely stored in a locked cabinet or box and out of the reach of children.
- Keep medicines in their original child-resistant containers and never in unsecured containers.
- Properly discard unfinished or unused medicines.
Laundry Packets
- Store laundry packets in their original containers and out of a child’s sight and reach.
- Do not let children handle laundry detergent packets.
Household Cleaning Supplies
- Keep chemicals and cleaning supplies safely stored in a locked cabinet or box and out of the reach of children.
- Keep household chemicals in their original child-resistant containers.
Button Cell or Coin Batteries
- Keep products with accessible batteries away from children if the battery compartments do not have a screw closure or if the compartment is damaged.
- Check the toys in your home to make sure battery compartments are secured.
- Do not allow children to play with or be in contact with button cell or coin batteries.
About the U.S. CPSC
The U.S. Consumer Product Safety Commission (CPSC) is charged with protecting the public from unreasonable risk of injury or death associated with the use of thousands of types of consumer products. Deaths, injuries, and property damage from consumer product-related incidents cost the nation more than $1 trillion annually. CPSC’s work to ensure the safety of consumer products has contributed to a decline in the rate of injuries associated with consumer products over the past 50 years.
Federal law prohibits any person from selling products subject to a Commission ordered recall or a voluntary recall undertaken in consultation with the CPSC.
For lifesaving information:
- Visit CPSC.gov.
- Sign up to receive our e-mail alerts.
- Follow us on Facebook, Instagram @USCPSC and Twitter @USCPSC.
- Report a dangerous product or a product-related injury on www.SaferProducts.gov.
- Call CPSC’s Hotline at 800-638-2772 (TTY 301-595-7054).
- Contact a media specialist.
We all have some kind of button battery in things we may not even think of. Most of us older folks have a hard time getting the back off of a device, but that doesn’t mean that your tech device is baby-proof or child resistant.
The copyrighted poster below is from the CPSC – Consumer Product Safety Commission. I borrowed for informational purposes.
Now we know some of the places that have those important sources of energy for our tech devices. But, how do we know whose body the lost lithium battery is lodged in?
The following block quote content is not from my personal knowledge base specific to battery buttons. Any time you see these signs- please do NOT give your child an old home remedy like a piece of bread or trying Ipecac. Do NOT do it. But follow the directions below even if you do not think the child or old enough to know better kid ingested something that is not food.
With so many families preparing for an SHTF event, we have lots and lots of battery-powered gizmos. These items may be a convenience that may advance us a few stages above the stone age, many of these save our lives or put someone in danger when in the wrong hands or the directions are not followed.
Remember: Many accidents are PREVENTABLE!
I got the following block quote safety information from eMedicineHealth. I have copied and pasted it for information purposes. Symptoms and Signs of Battery Ingestion (Swallowed Battery): Treatment (emedicinehealth.com)
Medical Author: Charles Patrick Davis, MD, PhD
Medically Reviewed on 8/25/2021Battery ingestion signs and symptoms unfortunately may not become obvious until the battery begins to harm tissue.
However, if the battery initially blocks the airway, difficulty breathing may be the first symptom of battery ingestion. Signs and symptoms of battery ingestion may include
- low-grade fever,
- irritability,
- drooling,
- abdominal pain,
- vomiting,
- gagging,
- rash, especially if the patient has a metal allergy (for example, skin reaction to nickel),
- blood in the stools,
- dark tarry stools, and
- difficulty breathing.
Symptoms and Signs of Battery Ingestion (Swallowed Battery): Treatment (emedicinehealth.com)
- Call 911 and poison control (1-800-222-1222), and transport the patient to an appropriate ER (child or adult). If possible, determine the type of battery swallowed.
I am going to leave it up to you to click that link above for a partial list of things that will be done in the ER before accidental ingestion occurs in your family. Unless you have Xray vision, your child will need an XRAY.
Part of preparedness for prepper families is to know how to prevent before an injury occurs.
I also have a disclaimer:
This post is not intended to provide medical advice: diagnose, treat, or prescribe. SEEK medical advice. This No Non-cents Nanna post is for informational informaiton only.
I hope you enjoyed the information is this post about poison control.
Until next time, I am Malika Bourne the No Non-cents Nanna reminding you to “Make Good Choices.”
BONUS
Now, don’t go getting smug on me because you only use “natural ingredients”… I’m going to briefly mentions some everyday items in your spice cupboard that in the wrong hands can cause grave harm. In an additional post TBA I will be more thorough. This is just a teaser…
The first resource below has more to do with lead poisoning in your herbs and spices. No Non-cents Nanna is working on this 2 to 3-post series. I have a ton of shocking information that you will want to know. (No the government is not planning on taking away your spices. Wait for it…)
The investigators tested 15 types of common spices, including black pepper, cumin, ginger powder, oregano, and paprika. They found 40 out of 126 tested products to contain enough heavy metals that could pose health threats to children.www.verywellhealth.com/spice-lead-exposure-5209991On January 13, 2018, the FDA issued an update to its 2013 draft risk profile on spices to include analysis of a two-year, nationwide study to collect data on the presence of Salmonella in retail packages that you would find in supermarkets, ethnic markets, discount stores, and on the internet. The data demonstrate that the prevalence of Salmonella in nine out of 11 types of retail spices in the U.S. was significantly lower than that for shipments of spice at import. Questions & Answers on Improving the Safety of Spices | FDA
…problem relates in part to poor or inconsistent use of appropriate controls to prevent contamination. Spice shipments from 79 countries were examined for Salmonella, and we found that 37 of the 79 countries had Salmonella-contaminated shipments, indicating that contamination of spice shipments with Salmonella is not limited to just a few source countries.
If your prepper family is planning on bugging out of the big city to live off the land – you’ve got a lot more thinking to do. A
You are delussion if you think that you will automatically be finding random milk and honey and goods weeds to eat will take a lot of book-reading with pictures and a great dealing of real experience prior to living like John the Baptist or Elija.. If you have that Red Dawn fantasy…you are only dreaming.
Before we get the first on the list below, honey I want to firmly state do NOT EVER give infants honey no matter how “natural” you believe it is. Honey is one of those things that you can find naturally occurring botulism in it. Babies’ systems are not ready to throw it off as people with bigger and more mature bodies can.
I have actually had a pediatric intensive care patient who had an auntie who used an old-home remedy on a fussy nephew. She put honey on a pacifier – the baby was completely paralyzed from botulism. That is the short version – I am dead serious. Currently, I don’t have a No Non-cents Nanna post on this.
Kidney beans are also in the list below. For those who love sensory boxes for our kiddos to explore: Do NOT put in raw kidney beans. If a child puts those beans in their mouths (and they will) without choking on them first kidney beans will poison them.
- Honey (Grayanotoxins): Bees collect nectar from flowers in order to create honey. If those flowers have a natural toxin, that toxin may end up in the honey from that beehive. One example is grayanotoxins, which plants such as rhododendrons and mountain laurel naturally produce. Eating honey with a high amount of this toxin can lead to “mad honey” poisoning, with symptoms such as nausea, vomiting, or dizziness. This type of poisoning is rare.
- Beans (Phytohaemagglutinin): Phytohaemagglutinin (PHA) is a lectin found in raw or undercooked beans. Lectins are proteins that bind to carbohydrates and some plants produce them as a natural defense mechanism. In canned and properly cooked kidney beans, the low levels of PHA won’t affect you. But at high levels in raw beans, PHA can lead to nausea, severe vomiting, and diarrhea. Soaking the beans for a minimum of 5 hours and then boiling them in fresh water for at least 30 minutes will remove and destroy this toxin.
- Mushrooms (Mushroom toxins): It’s well known that some mushrooms are toxic. Depending on the type of mushroom you eat, you could experience milder reactions like nausea or diarrhea. More severe reactions include coma and death.
- Stone fruit, such as peaches or apricots (Amygdalin): Amygdalin, also called laetrile, is a natural chemical found in the seeds of apricots, bitter almonds, apples, peaches, and plums. The chemical is not found in the fruit itself and accidentally eating a seed or pit will not harm you. However, consuming a large amount of the seeds or pits can be problematic because enzymes in your intestines can turn amygdalin into cyanide and cause cyanide poisoning.
I saved the best for last. If you stuck with me in this post you are going to want to hear this information.
I admit that I can be a Negative Nelly dashing some Myths about Natural Foods. I’ve lost track of the years or decades that I have heard shock, disbelieve, defensiveness then anger when someone partially learns that The FDA or some “evil” government agency is picking on our right to eat “Natural Foods”,
I am going to tell you flat-out that the U. S. government is NOT banning “natural foods like herbs or essential oils.” Recalling is not the same thing as banning. Get that straight. I often quote for U. S. Governmental Agencies so you can get the facts in context from the original source. Not just my opinion.
Please note disclaimers. This post is for informational purposes only. It is not intended to take the place of medical advice from our own medical practitioner.
The problems were recalls are issued over non-compliant safety packaging. or contamination. Whether or not you want to believe this, even “natural” plant products can be extremely toxic if used in greater amounts than should be. Many people think that “if a small amount is good for you – then more must be better.”
Yes, you can overdose on herbs, spices, and extracts: Let’s start with 4. More will be compiled in a TBA No Non-cents Nanna post. Until then check out this article for more details – hints below:
Kitchen Surprises and Cautions (poison.org)
- Vanilla;
- Poppy;
- Nutmeg;
- Oil of Wintergreen
Is it true that….
- Enough vanilla extract can make you drunk?
- Poppy seeds contain opium?
- A lot of nutmeg is like a little PCP?
- Oil of wintergreen can cause an aspirin overdose?
Yes, all of these statements are true, though none of these foods and flavorings is dangerous to use as recommended.
Is it true that….
- Enough vanilla extract can make you drunk?
- Poppy seeds contain opium?
- A lot of nutmeg is like a little PCP?
- Oil of wintergreen can cause an aspirin overdose?
All of these statements are true, though none of these foods and flavorings is dangerous to use as recommended. Let’s review some kitchen poison safety tips.
According to Rose Ann Gould Soloway, RN, BSN, MSEd, DABAT emerita, Clinical Toxicologist…
It’s important to keep safety in mind even when using ordinary kitchen ingredients. Use only recommended amounts in recipes. Lock up ingredients that might be harmful if children swallow too much. And, as always, help from Poison Control right away if you suspect that someone has swallowed too much of anything. Even though you’re baking or partying, Poison Control guidance is available 24 hours a day. Use the webPOISONCONTROL® online tool for guidance or call Poison Control at 1-800-222-1222 to help you through any poison emergency.
WebSome ordinary kitchen ingredients can be harmful if children swallow large amounts. Examples include alcohol-based flavoring extracts, oil of wintergreen, and nutmeg. Poppy …
Views: 225